Written by: Molly M. Eggleston, MPH, CPH, MCHES, MIDAS Project Coordinator, Public Health Dynamics Laboratory
Copy editors: Linda S. Duchak, EdM, MCHES, Associate Director, and Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
People are neither perfectly informed nor perfectly rational. In epidemics, individuals do not always make logical health decisions to protect themselves and others. Realistic modeling of human behavior in the context of infectious disease allows public health practitioners to prepare for likely reactions to and spread of contagion.
Human behavior can affect the course of an epidemic through several mechanisms. Vaccine acceptance, work absenteeism, adoption of protective measures, isolation, and compliance with containment strategies and hygiene advice are among a wide range of personal health choices that influence epidemic dynamics.
Modeling simplifies real systems, such as waves of an epidemic, into a representation using a computer program. A model allows researchers and practitioners to test interventions that often cannot be tried on a real population.1 Developing realistic models of individual behavior can help forecast epidemic processes and better inform preparedness policy options. For example, a simulation of behavior of a population with emotions, attitudes, and behaviors can help inform risk communication campaigns during emerging epidemics. An understanding of individual’s compliance with government directives can assess the effect of various interventions.
Computational models of infectious disease hold great potential for studying the interactions between epidemic dynamics and efforts to reduce the impact. These efforts, known as mitigation strategies can include vaccination, anti-viral drugs, social distancing, and school closure policies.
Modeling people’s health behavior is a tool with value for many public health professionals. It can determine which course of action is likely to produce the desired health behavior in a population. Modeling human behavior is a strategic tool for planning for infectious diseases, as well as other health risks.
Citation: 1. Agent-Based and Individual-Based Modeling: A practical introduction, Steven F Railsback and Volker Grimm, Princeton University Press, 2012
Tuesday, November 26, 2013
Wednesday, October 30, 2013
ACA Implementation: Welcome to the Marketplace
Written by: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center
Copy editor: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
 On October 1, 2013, enrollment began for the Marketplaces under the Affordable Care Act (ACA) for coverage beginning on January 1, 2014. Signed into law in 2010, the ACA makes critical changes to health insurance in the United States. Some of the ACA changes (extending health insurance coverage of children until age 26 on parents’ insurance plans, for example) took effect in 2010. In January 2014, the most important changes go into effect.
On October 1, 2013, enrollment began for the Marketplaces under the Affordable Care Act (ACA) for coverage beginning on January 1, 2014. Signed into law in 2010, the ACA makes critical changes to health insurance in the United States. Some of the ACA changes (extending health insurance coverage of children until age 26 on parents’ insurance plans, for example) took effect in 2010. In January 2014, the most important changes go into effect.
A key component of the ACA is to increase the accessibility of health insurance for all Americans. To do this, the Health Insurance Marketplaces were established. The Marketplace in each state is made up of private health insurance plans that must cover a basic set of benefits, including preventative care (such as screenings and check-ups), other doctor visits, prescriptions, hospitalization, family planning and maternity care. It provides people with different plan options and costs. Approximately half of the states are operating their own Marketplace; the federal government is operating the Marketplace in the 26 states that opted not to create their own.
People who purchase insurance through the marketplace may be eligible for tax credits or a cost-sharing reduction, depending upon their income. Income also determines how much people have to pay for copays, co-insurance and deductibles. In some states people whose annual incomes are below 138% of the Federal Poverty Level ($15,856) may be eligible for premium-free coverage through Medicaid. People who can afford to purchase insurance may face a penalty fee if they decide not to buy it.
Copy editor: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
 On October 1, 2013, enrollment began for the Marketplaces under the Affordable Care Act (ACA) for coverage beginning on January 1, 2014. Signed into law in 2010, the ACA makes critical changes to health insurance in the United States. Some of the ACA changes (extending health insurance coverage of children until age 26 on parents’ insurance plans, for example) took effect in 2010. In January 2014, the most important changes go into effect.
On October 1, 2013, enrollment began for the Marketplaces under the Affordable Care Act (ACA) for coverage beginning on January 1, 2014. Signed into law in 2010, the ACA makes critical changes to health insurance in the United States. Some of the ACA changes (extending health insurance coverage of children until age 26 on parents’ insurance plans, for example) took effect in 2010. In January 2014, the most important changes go into effect.A key component of the ACA is to increase the accessibility of health insurance for all Americans. To do this, the Health Insurance Marketplaces were established. The Marketplace in each state is made up of private health insurance plans that must cover a basic set of benefits, including preventative care (such as screenings and check-ups), other doctor visits, prescriptions, hospitalization, family planning and maternity care. It provides people with different plan options and costs. Approximately half of the states are operating their own Marketplace; the federal government is operating the Marketplace in the 26 states that opted not to create their own.
People who purchase insurance through the marketplace may be eligible for tax credits or a cost-sharing reduction, depending upon their income. Income also determines how much people have to pay for copays, co-insurance and deductibles. In some states people whose annual incomes are below 138% of the Federal Poverty Level ($15,856) may be eligible for premium-free coverage through Medicaid. People who can afford to purchase insurance may face a penalty fee if they decide not to buy it.
Thursday, October 3, 2013
Pennsylvania has a Poor National Standing for Infant Mortality
Written by: Linda S. Duchak, EdM, MCHES, Associate Director, Pennsylvania Public Health Training Center
Copy editor: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
In the U.S., for every 1,000 babies born, about 6 die before age 1. In Pennsylvania, for every 1,000 babies born, about 7 die before they reach age 1 (2010). Only 11 states in the U.S. had higher rate of infant mortality than Pennsylvania.
Infant mortality is defined as the death of an infant before his or her first birthday. The infant mortality rate (IMR) measures this occurrence per 1,000 live births. In addition to being a key marker of maternal and child health, the IMR has been called the most sensitive indicator of overall societal health.
In the United States, substantial progress has been made over the last 50 years in reducing the IMR. Yet with an IMR of 6.05 in 2011, the U.S. still has a relatively poor global standing. In 2010, the United States ranked 32nd among the 34 nations of the Organization for Economic Cooperation and Development in infant mortality with an overall IMR three times that of the countries with the lowest IMRs. The main reason that the U.S. IMR remains higher than that of European nations is because the U.S. has a high percentage of preterm births (12%).
Infant mortality is divided into two age periods: neonatal (birth–27 days) and post-neonatal (28–364 days). Approximately two-thirds of all infant deaths occur in the neonatal period and are caused by complications arising from low birth weight, birth defects, maternal health, preterm birth, complications of labor and delivery, and lack of access to appropriate care at the time of delivery. These problems can be linked to a complex group of conditions, including systematic inequality and lack of access to care.
Racial and geographic disparities remain persistent. Non-Hispanic black infants continue to die at nearly twice the rate of non-Hispanic white infants. Additionally, preterm-related causes of death among black infants occur at a rate three times greater than that of white infants. Geographically, Pennsylvania is included with a majority of southern states in the top quartile for infant mortality.
Further reduction of preventable infant deaths remains a challenge. Prevention of infant deaths should begin in the preconception period; opportunities are available to improve the health of mothers and thus avoid preventable infant deaths. The rates of preterm birth, including rates of late preterm birth (births between 34 and 36 weeks of gestation) and elective preterm delivery, need to be reduced. Opportunities exist to reduce the mortality rate among infants born preterm by addressing key risk factors such as maternal smoking, drinking, drug use, and chronic maternal health problems such as high blood pressure and diabetes. Many very low birth weight infants in the United States are not born in hospitals that have level III neonatal intensive-care units, which have been shown to significantly reduce mortality, indicating a need to increase access to high quality care.
Source: Morbidity and Mortality Weekly Report, August 9, 2013 / 62(31);625-628.
Copy editor: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
In the U.S., for every 1,000 babies born, about 6 die before age 1. In Pennsylvania, for every 1,000 babies born, about 7 die before they reach age 1 (2010). Only 11 states in the U.S. had higher rate of infant mortality than Pennsylvania.
Infant mortality is defined as the death of an infant before his or her first birthday. The infant mortality rate (IMR) measures this occurrence per 1,000 live births. In addition to being a key marker of maternal and child health, the IMR has been called the most sensitive indicator of overall societal health.
In the United States, substantial progress has been made over the last 50 years in reducing the IMR. Yet with an IMR of 6.05 in 2011, the U.S. still has a relatively poor global standing. In 2010, the United States ranked 32nd among the 34 nations of the Organization for Economic Cooperation and Development in infant mortality with an overall IMR three times that of the countries with the lowest IMRs. The main reason that the U.S. IMR remains higher than that of European nations is because the U.S. has a high percentage of preterm births (12%).
Infant mortality is divided into two age periods: neonatal (birth–27 days) and post-neonatal (28–364 days). Approximately two-thirds of all infant deaths occur in the neonatal period and are caused by complications arising from low birth weight, birth defects, maternal health, preterm birth, complications of labor and delivery, and lack of access to appropriate care at the time of delivery. These problems can be linked to a complex group of conditions, including systematic inequality and lack of access to care.
Racial and geographic disparities remain persistent. Non-Hispanic black infants continue to die at nearly twice the rate of non-Hispanic white infants. Additionally, preterm-related causes of death among black infants occur at a rate three times greater than that of white infants. Geographically, Pennsylvania is included with a majority of southern states in the top quartile for infant mortality.
Further reduction of preventable infant deaths remains a challenge. Prevention of infant deaths should begin in the preconception period; opportunities are available to improve the health of mothers and thus avoid preventable infant deaths. The rates of preterm birth, including rates of late preterm birth (births between 34 and 36 weeks of gestation) and elective preterm delivery, need to be reduced. Opportunities exist to reduce the mortality rate among infants born preterm by addressing key risk factors such as maternal smoking, drinking, drug use, and chronic maternal health problems such as high blood pressure and diabetes. Many very low birth weight infants in the United States are not born in hospitals that have level III neonatal intensive-care units, which have been shown to significantly reduce mortality, indicating a need to increase access to high quality care.
Source: Morbidity and Mortality Weekly Report, August 9, 2013 / 62(31);625-628.
Wednesday, August 28, 2013
What is the Community Guide?
Written by: Linda S. Duchak, EdM, MCHES, Associate Director, Pennsylvania Public Health Training Center
Copy editors: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
The Guide to Community Preventive Services (Community Guide), a collection of evidence-based findings and recommendations grounded in systematic reviews, is a useful tool to inform public health activities. Development of the guide is overseen by the Community Preventive Services Task Force (Task Force), renowned for its expertise in public health research, practice, prevention, and policy.
The Community Guide informs public health program and policy development as well as priorities for funding by providing descriptive information, estimated costs, and potential return on investment of community preventive services, programs, and policies that have been proven to be effective. Findings and recommendations focus on a broad range of topics, including adolescent health, asthma, birth defects, chronic disease, emergency preparedness, health equity, mental health, oral health, tobacco, violence, and worksite health promotion. Public health practitioners based at state and local health departments; board of health members, policymakers and legislators, health plans, hospital and their community advisory groups, educators and school administrators, city and county planners, social service agencies and organizations, and clinicians and community health centers use the Community Guide to address public health issues.
The findings and recommendations are based on evidence from systematic reviews found in the scientific literature. The reviews evaluate the evidence by:
The Community Guide is in the public domain and available online at www.thecommunityguide.org. Contact us at paphtc@pitt.edu (Western PA) or paphtc@drexel.edu (Eastern PA) if you need help developing public health programs or policies.
Copy editors: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
 |
| www.thecommunityguide.org |
- Building a public health program or developing policy?
- Considering research to close a gap in an area of need?
The Guide to Community Preventive Services (Community Guide), a collection of evidence-based findings and recommendations grounded in systematic reviews, is a useful tool to inform public health activities. Development of the guide is overseen by the Community Preventive Services Task Force (Task Force), renowned for its expertise in public health research, practice, prevention, and policy.
The Community Guide informs public health program and policy development as well as priorities for funding by providing descriptive information, estimated costs, and potential return on investment of community preventive services, programs, and policies that have been proven to be effective. Findings and recommendations focus on a broad range of topics, including adolescent health, asthma, birth defects, chronic disease, emergency preparedness, health equity, mental health, oral health, tobacco, violence, and worksite health promotion. Public health practitioners based at state and local health departments; board of health members, policymakers and legislators, health plans, hospital and their community advisory groups, educators and school administrators, city and county planners, social service agencies and organizations, and clinicians and community health centers use the Community Guide to address public health issues.
The findings and recommendations are based on evidence from systematic reviews found in the scientific literature. The reviews evaluate the evidence by:
- Analyzing all available evidence on what works to promote health and prevent disease, injury, and disability;
- Assessing the economic benefits of the interventions found to be effective; and
- Identifying where more evidence is needed.
The Community Guide is in the public domain and available online at www.thecommunityguide.org. Contact us at paphtc@pitt.edu (Western PA) or paphtc@drexel.edu (Eastern PA) if you need help developing public health programs or policies.
Wednesday, July 24, 2013
The Health Benefits of Engaging in Art and Civic Programs
Written by: Jason Flatt, PhD, MPH, Postdoctoral Fellow, University of Pittsburgh
Copy editor: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
Art and civic programs, including visual, musical and other creative art programs, are something that can be appreciated and enjoyed throughout one’s lifespan. Who would have thought that being active in the arts would have health benefits? Several studies have shown that engaging in artistic endeavors can help to relieve negative symptoms associated with cancer, may promote positive mental health, relieve emotional distress and pain, help with minimizing the stigma associated with a debilitating disease and increase opportunities for enjoyable social interactions (Carnic & Chatterjee, 2013; Stuckey & Nobel, 2010). Research has also shown that participating in various types of art programs have benefits for older adults with dementia.
A recent project looked at the benefits of visiting an art museum and participating in art-making for older adults with dementia and their caregivers. Four focus groups were conducted with participants at the end of their visit to the Andy Warhol museum, and participants also completed a very short satisfaction survey. Participants reported that they thoroughly enjoyed the experience, especially because of the opportunities to socialize with others, be creative, and feel accepted by others. Caregivers also enjoyed the experience and mentioned how art provided them and their family member with an opportunity for mental stimulation and to reminisce about the past.
This highlights the need for a greater connection between public health and art and civic programs, such as museums and other recreational activities. These programs have a lot of potential benefits for health, and there is a need for further exploration of the benefits of being engaged in art and civic programs.
References:
Carnic, P.M., & Chatterjee, H.J. (2013). Museums and art galleries as partners for public health interventions. Perspectives in Public Health, 133(1), 66-71. doi: 10.1177/1757913912468523
Stuckey, H. L., & Nobel, J. (2010). The connection between art, healing, and public health: a review of current literature. American Journal of Public Health, 100(2), 254-263. doi: 10.2105/AJPH.2008.156497
Copy editor: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
Art and civic programs, including visual, musical and other creative art programs, are something that can be appreciated and enjoyed throughout one’s lifespan. Who would have thought that being active in the arts would have health benefits? Several studies have shown that engaging in artistic endeavors can help to relieve negative symptoms associated with cancer, may promote positive mental health, relieve emotional distress and pain, help with minimizing the stigma associated with a debilitating disease and increase opportunities for enjoyable social interactions (Carnic & Chatterjee, 2013; Stuckey & Nobel, 2010). Research has also shown that participating in various types of art programs have benefits for older adults with dementia.
A recent project looked at the benefits of visiting an art museum and participating in art-making for older adults with dementia and their caregivers. Four focus groups were conducted with participants at the end of their visit to the Andy Warhol museum, and participants also completed a very short satisfaction survey. Participants reported that they thoroughly enjoyed the experience, especially because of the opportunities to socialize with others, be creative, and feel accepted by others. Caregivers also enjoyed the experience and mentioned how art provided them and their family member with an opportunity for mental stimulation and to reminisce about the past.
This highlights the need for a greater connection between public health and art and civic programs, such as museums and other recreational activities. These programs have a lot of potential benefits for health, and there is a need for further exploration of the benefits of being engaged in art and civic programs.
| Silk Screen Paintings by Persons with Dementia and their Caregivers |
References:
Carnic, P.M., & Chatterjee, H.J. (2013). Museums and art galleries as partners for public health interventions. Perspectives in Public Health, 133(1), 66-71. doi: 10.1177/1757913912468523
Stuckey, H. L., & Nobel, J. (2010). The connection between art, healing, and public health: a review of current literature. American Journal of Public Health, 100(2), 254-263. doi: 10.2105/AJPH.2008.156497
Friday, June 21, 2013
The Importance of Social Media During a Crisis
Written by: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
Copy editor: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center
Social media is an interactive online communication method that offers the ability to provide immediate information, create dynamic relationships with the community, and disseminate information to media outlets. While some people view social media as a form of online entertainment, public health professionals are recognizing the importance of social media during a crisis.
According to 2013 trend data from the Pew Internet & American Life Project,1 84 percent of the United States population uses the Internet with 67 percent of those users accessing social network site such as Facebook, LinkedIn, or Google Plus. These percentages are rapidly growing as ownership of mobile devices such as smart phones and tablets continue to skyrocket in popularity.
Social media is emerging as the overwhelming driver of news. During a crisis, over two-thirds of all mainstream media outlets have acknowledged that they seek out information from the responding agency through social media.2 As a responding agency during a crisis, it is important to engage this audience as they seek out more information. If the agency is not engaging, the media outlets will turn to other social media sources for information. It is the 21st century equivalent to not returning a reporter’s phone calls.
With such a large importance being placed on social media, 68 percent of the nation's county emergency management agencies, and 85 percent of the nation's local response agencies reported using social media in 2012.3 The primary barriers to effective implementation of social media in emergency management agencies have been noted as a lack of dedicated personnel and the lack of commitment from senior leadership. In order to overcome these barriers, social media needs to become an embedded element of a communications plan with clearly established goals of social media usage. As senior management becomes more comfortable about broader support of social media as an important communications method, the support for personnel and percentage of social media usage should increase.
Social media has become an essential communications method and public health professionals are recognizing its importance. As 2013 progresses, social media will continue to play an important role in crisis management and all aspects of public health can benefit from learning how to use social media to meet public health goals.
[1] Pew Internet & American Life Project - http://pewinternet.org/
[2] Crisis Emergency and Risk Communication 2012 Edition. U.S. Department of Health and Human Services Center for Disease Control and Prevention. Page 259. http://emergency.cdc.gov/cerc/pdf/CERC_2012edition.pdf
[3] Social Media in the Emergency Management Field 2012 Survey Results. CNA Analysis & Solutions. Page 26. http://www.cna.org/sites/default/files/research/SocialMedia_EmergencyManagement.pdf
Copy editor: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center
Social media is an interactive online communication method that offers the ability to provide immediate information, create dynamic relationships with the community, and disseminate information to media outlets. While some people view social media as a form of online entertainment, public health professionals are recognizing the importance of social media during a crisis.
According to 2013 trend data from the Pew Internet & American Life Project,1 84 percent of the United States population uses the Internet with 67 percent of those users accessing social network site such as Facebook, LinkedIn, or Google Plus. These percentages are rapidly growing as ownership of mobile devices such as smart phones and tablets continue to skyrocket in popularity.
Social media is emerging as the overwhelming driver of news. During a crisis, over two-thirds of all mainstream media outlets have acknowledged that they seek out information from the responding agency through social media.2 As a responding agency during a crisis, it is important to engage this audience as they seek out more information. If the agency is not engaging, the media outlets will turn to other social media sources for information. It is the 21st century equivalent to not returning a reporter’s phone calls.
With such a large importance being placed on social media, 68 percent of the nation's county emergency management agencies, and 85 percent of the nation's local response agencies reported using social media in 2012.3 The primary barriers to effective implementation of social media in emergency management agencies have been noted as a lack of dedicated personnel and the lack of commitment from senior leadership. In order to overcome these barriers, social media needs to become an embedded element of a communications plan with clearly established goals of social media usage. As senior management becomes more comfortable about broader support of social media as an important communications method, the support for personnel and percentage of social media usage should increase.
Social media has become an essential communications method and public health professionals are recognizing its importance. As 2013 progresses, social media will continue to play an important role in crisis management and all aspects of public health can benefit from learning how to use social media to meet public health goals.
[1] Pew Internet & American Life Project - http://pewinternet.org/
[2] Crisis Emergency and Risk Communication 2012 Edition. U.S. Department of Health and Human Services Center for Disease Control and Prevention. Page 259. http://emergency.cdc.gov/cerc/pdf/CERC_2012edition.pdf
[3] Social Media in the Emergency Management Field 2012 Survey Results. CNA Analysis & Solutions. Page 26. http://www.cna.org/sites/default/files/research/SocialMedia_EmergencyManagement.pdf
Wednesday, May 29, 2013
Towards Religious Competency for Health Professionals
Written by: Eleanor Lippmann, MPH
Copy editors: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
Copy editors: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
An elderly Hindu woman presents at a city health clinic with
her teenage granddaughter acting as an interpreter. The teenager explains that her grandmother
has been sad and reclusive for the past couple of months because she has pain
in her hands. She has been unable to do
her normal activities like working in her garden and cooking for her
family. The doctor examines the elderly
woman and finds that she is suffering from severe arthritis in her hands. He offers to give her a prescription to treat
the pain so that she can return to doing the things that she loves. When the teenager translates this
information, the elderly woman just shakes her head and slumps in her chair.
The teenager explains
to the doctor that in Hinduism, there is a central belief in the doctrine of
karma, the law of cause and effect. Every thought, word, and action accumulates karma, which can affect
current and future lives, including health and well-being. Her grandmother believes that the pain in her
hands is a natural consequence for something she has done in a past life. Rather than treat the pain, she sees this as
an opportunity to progress spiritually. How
can the doctor respect her choice while also giving her the highest quality of
care?
Understanding the reasoning behind a patient’s medical
decisions is critical in clinical practice, for both better prevention and
treatment. The Co-PI of the PA Public
Health Training Center, Jennifer Kolker, explains, "So just like we ask
somebody about their marital status, or we ask about sexual activity, or we ask
about employment, we should be able to ask questions about whether or not they
are member of a faith, how adherent to a faith they are and are there things
about their faith that a clinician might need to know in treating them?"
To better understand the intersection of religion and
health, providers may need to consider the following questions:
- How much does a particular
religion inform the patient’s health decisions?
- What are the long-term
effects of this patient turning down treatment?
- In this particular
religion, is there a more effective way to communicate information about
treatment?
- Who, in this religious
community, may be a good resource for health practitioners to contact if
they are having trouble giving care to a patient?
While this particular scenario features Hindus, a similar
scenario could be described for Catholics, Jews, Buddhists – people of many
different faiths. And while it would be
impossible for providers to be competent in every religion, it is their responsibility
to ask the right questions in order to effectively treat their patients.
Wednesday, April 24, 2013
The Competencies of Leadership
Written by: Gerald Barron, MPH, Deputy Director, University of Pittsburgh Graduate School of Public Health Center for Public Health Practice
Copy editor: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
Leadership is important. Governmental agencies, non-profit organizations, and businesses all have been shown to be better able to meet their mission and accomplish their goals when they have strong leadership. Therefore, it is important to understand what is needed to be a good leader. Who are leaders? A leader is someone you would follow to a place you would not go on your own. In the follower’s estimation, this is a better place. The most important component of the leader-follower relationship is trust. It is important that we trust our leaders or we won’t follow them. How is this trust developed? It’s developed by the leader exhibiting the following competencies:
Creates and Embraces a Vision – Envisions the future by creating an exciting, compelling, and credible possibility
Takes and Builds Accountability – Acts in a responsible way
Demonstrates Resolve and Decisiveness – Makes decisions about what to do with courage and firm determination
Self Regulates – Resists or delays any impulses, drives, or temptations to act which may detract from the achievement of goals
Self-Knowledge – Recognizes his/hers own skills, abilities, emotions, preferences, biases, and predispositions
Empathetic/Compassionate – Has a full range of authentic emotional expression that enables the addressing of one’s own needs as well as the needs of others
Active Listening – Pays concentrated attention to what someone else is saying as well as paying attention to what is motivating or influencing the other person
Communicates Messages Effectively – Communicates messages effectively using words, symbolism and personal example
Motivates and Empowers People – Understands how and why people feel and act as they do, whether motivated by enlightened self-interest, team interest, or organizational interest
Timing of Action – Demonstrates an appropriate sense of timing for announcements, decisions, actions, and in-actions
Copy editor: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
Leadership is important. Governmental agencies, non-profit organizations, and businesses all have been shown to be better able to meet their mission and accomplish their goals when they have strong leadership. Therefore, it is important to understand what is needed to be a good leader. Who are leaders? A leader is someone you would follow to a place you would not go on your own. In the follower’s estimation, this is a better place. The most important component of the leader-follower relationship is trust. It is important that we trust our leaders or we won’t follow them. How is this trust developed? It’s developed by the leader exhibiting the following competencies:
Creates and Embraces a Vision – Envisions the future by creating an exciting, compelling, and credible possibility
Takes and Builds Accountability – Acts in a responsible way
Demonstrates Resolve and Decisiveness – Makes decisions about what to do with courage and firm determination
Self Regulates – Resists or delays any impulses, drives, or temptations to act which may detract from the achievement of goals
Self-Knowledge – Recognizes his/hers own skills, abilities, emotions, preferences, biases, and predispositions
Empathetic/Compassionate – Has a full range of authentic emotional expression that enables the addressing of one’s own needs as well as the needs of others
Active Listening – Pays concentrated attention to what someone else is saying as well as paying attention to what is motivating or influencing the other person
Communicates Messages Effectively – Communicates messages effectively using words, symbolism and personal example
Motivates and Empowers People – Understands how and why people feel and act as they do, whether motivated by enlightened self-interest, team interest, or organizational interest
Timing of Action – Demonstrates an appropriate sense of timing for announcements, decisions, actions, and in-actions
Tuesday, March 26, 2013
Digging into Shale Gas and its Effects on Public Health
Copy editors: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
 |
|
Figure 1. PA
Production and Waste From Unconventional Wells:
July 2012 to December 2012. Data source: PA DEP. Map: FracTracker.org |
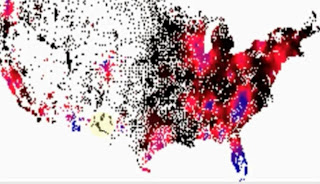
 Today’s natural gas is not found in shallow pockets tapped by drillers generations ago. It is tightly packed in deep shale deposits requiring considerable effort to extract it.
Today’s natural gas is not found in shallow pockets tapped by drillers generations ago. It is tightly packed in deep shale deposits requiring considerable effort to extract it.Drillers pump millions of gallons of water and chemicals underground to hydraulically fracture the shale and release the gas. The process involves hundreds of truck trips to deliver the site materials and haul away the waste. Blowouts, fires, and traffic incidents add to burdens already shouldered by rural emergency responders and health care practitioners. Truck trips, diesel-powered compressors, and silica sand used during hydraulic fracturing also worsen air quality. Waste water improperly injected into deep wells (See Figure 1) has induced earthquakes (~4.0 magnitude).[1]
Despite these potential health risks, public health professionals’ input was missing from early regulatory discussions about the benefits and costs of shale gas extraction.[2] While the public health workforce has weighed in more recently, additional issues need action. Most importantly, chemical mixtures returned to the surface after drilling should be actively monitored. Private drinking water wells in the vicinity need pre- and post-water quality tests. The air, water, and soil pathways to potential human contamination exposure require systematic study. And finally, micro-seismic monitoring of hydraulic fractures and wastewater injection should be conducted. Responsiveness to the results of these studies can reduce the potential environmental health impacts posed by this industry today and in the future.
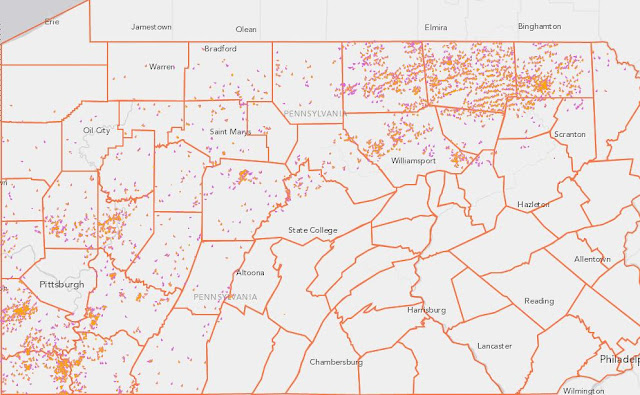 |
|
Figure 2. Drilled
(orange) and permitted (pink) unconventional wells in PA as of 1-4-13.
Data source: PA DEP. Map: FracTracker.org |
1. For a comprehensive list of health concerns associated with unconventional natural gas extraction, see Korfmacher, Jones, Malone, and Vinci (2013).
2. Goldstein BD, Kriesky J, Pavliakova B. (2012). Missing from the Table: Role of the Environmental Public Health Community in Governmental Advisory Commissions Related to Marcellus Shale Drilling. Environ Health Perspect, 120(4): pp. 483–486.
Tuesday, February 26, 2013
Flu Activity Declines Nationally and in Pennsylvania
Written by: Charles Vukotich, Jr. MS, Senior Project Manager, University of Pittsburgh Social Mixing And Respiratory Transmission in Schools (SMART in Schools)
Copy editors: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
The 2012-2013 flu season has proved to be one of the worst years for influenza in recent history. It was the second worst flu season since 2003 and one of the earliest flu seasons on record, with the exception of 2009 (H1N1). Flu activity started in late November. This was earlier than the 2003 season, which was mostly over by January. As of the current time, flu is still widespread in 38 states.
Influenza started in the south and moved to Pennsylvania by December. It was widespread in all 50 states and peaked during the last week of December through mid-January. Pennsylvania peaked in the second week of January at ~6,000 cases. By comparison, the 2009 H1N1 season peak was ~8,000 cases. Typical seasons have recently peaked at ~2,500 cases or less. The flu has affected those 65+ most (22.9% of cases), but also substantially affected the 25-49 age group (22.6%). The flu this season is primarily Flu A (90% of cases), and of the H3N2 strain.
While much is known about how flu spreads, we still don’t know what the best practice prevention methods are (such as school closures). The SMART in Schools program is working to better understand how social networks affect flu transmission. You can help by participating in a brief online survey and be entered into a weekly drawing for an Amazon or iTunes gift card. The anonymous survey takes 15 to 45 minutes to complete and is open to any resident of the United States.
For more flu information, visit www.cdc.gov/flu/.
Copy editors: Jennifer Kolker, MPH, Co-Principal Investigator, Pennsylvania Public Health Training Center; Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
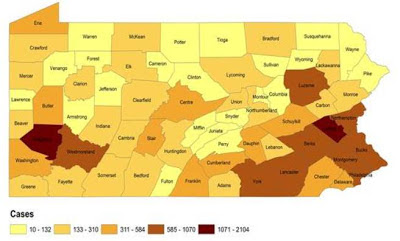 |
| Distribution of flu cases reported in Pennsylvania this season by county, 10/02/12 - 01/26/2013 (n=30,286) Source: PA Department of Health |
The 2012-2013 flu season has proved to be one of the worst years for influenza in recent history. It was the second worst flu season since 2003 and one of the earliest flu seasons on record, with the exception of 2009 (H1N1). Flu activity started in late November. This was earlier than the 2003 season, which was mostly over by January. As of the current time, flu is still widespread in 38 states.
Influenza started in the south and moved to Pennsylvania by December. It was widespread in all 50 states and peaked during the last week of December through mid-January. Pennsylvania peaked in the second week of January at ~6,000 cases. By comparison, the 2009 H1N1 season peak was ~8,000 cases. Typical seasons have recently peaked at ~2,500 cases or less. The flu has affected those 65+ most (22.9% of cases), but also substantially affected the 25-49 age group (22.6%). The flu this season is primarily Flu A (90% of cases), and of the H3N2 strain.
While much is known about how flu spreads, we still don’t know what the best practice prevention methods are (such as school closures). The SMART in Schools program is working to better understand how social networks affect flu transmission. You can help by participating in a brief online survey and be entered into a weekly drawing for an Amazon or iTunes gift card. The anonymous survey takes 15 to 45 minutes to complete and is open to any resident of the United States.
For more flu information, visit www.cdc.gov/flu/.
Lab positive flu cases reported in Pennsylvania this season (as of week 5) compared to the last six seasons
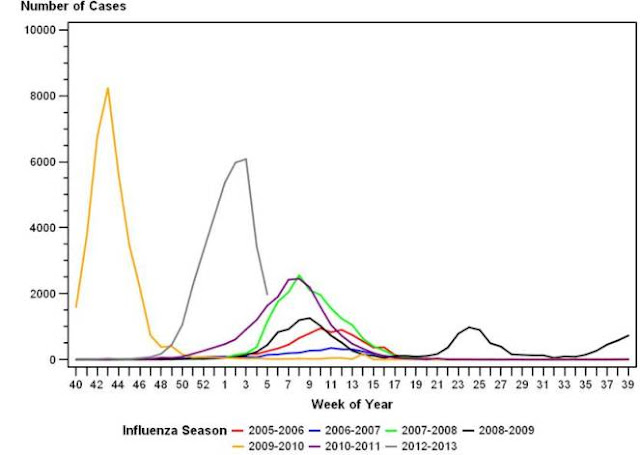 |
| Source: PA Department of Health |
Wednesday, January 23, 2013
New Year, New Style
 Written by: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training Center
Written by: Kurt Holliday, Communications Specialist, Pennsylvania Public Health Training CenterThe new year is here and it brought some new style to our communications. The Training Center recently launched a variety of new ways for you to stay informed about the latest workshops, distance education opportunities, conferences throughout Pennsylvania and the nation, and more. You will now spend less time searching for public health events, continuing education, and industry news and more time enjoying other things.
Ways to Follow Us
Web site - Creating an account is easy. Go to www.paphtc.pitt.edu and click the Create Account button. After creating an account, you gain access to all of its features.
E-mail - After creating an account, check that you would like to receive PA Training Alerts. You can update e-mail preferences by logging in, clicking on the My Info tab, and clicking on Change Info.Facebook - Have a Facebook account? Like us on Facebook
Twitter - Tweeting on Twitter? @PAPHTC
Subscribe to:
Posts (Atom)